Mechanical Engineering Technology (MET) undergraduate students had the opportunity to help develop low-cost medical devices for newborn patients in low- and middle-income countries (LMICs) through a capstone project during the 2023-24 academic year.
Paul Yearling, an associate clinical professor originally from IUPUI’s Mechanical Engineering Technology program and now a part of Purdue University in Indianapolis, has formed a collaborative relationship with Osayame Ekhaguere from Riley Hospital for Children in Indianapolis. Together they have created a robust undergraduate capstone project that will solve real-world healthcare engineering problems in countries with limited resources and access.
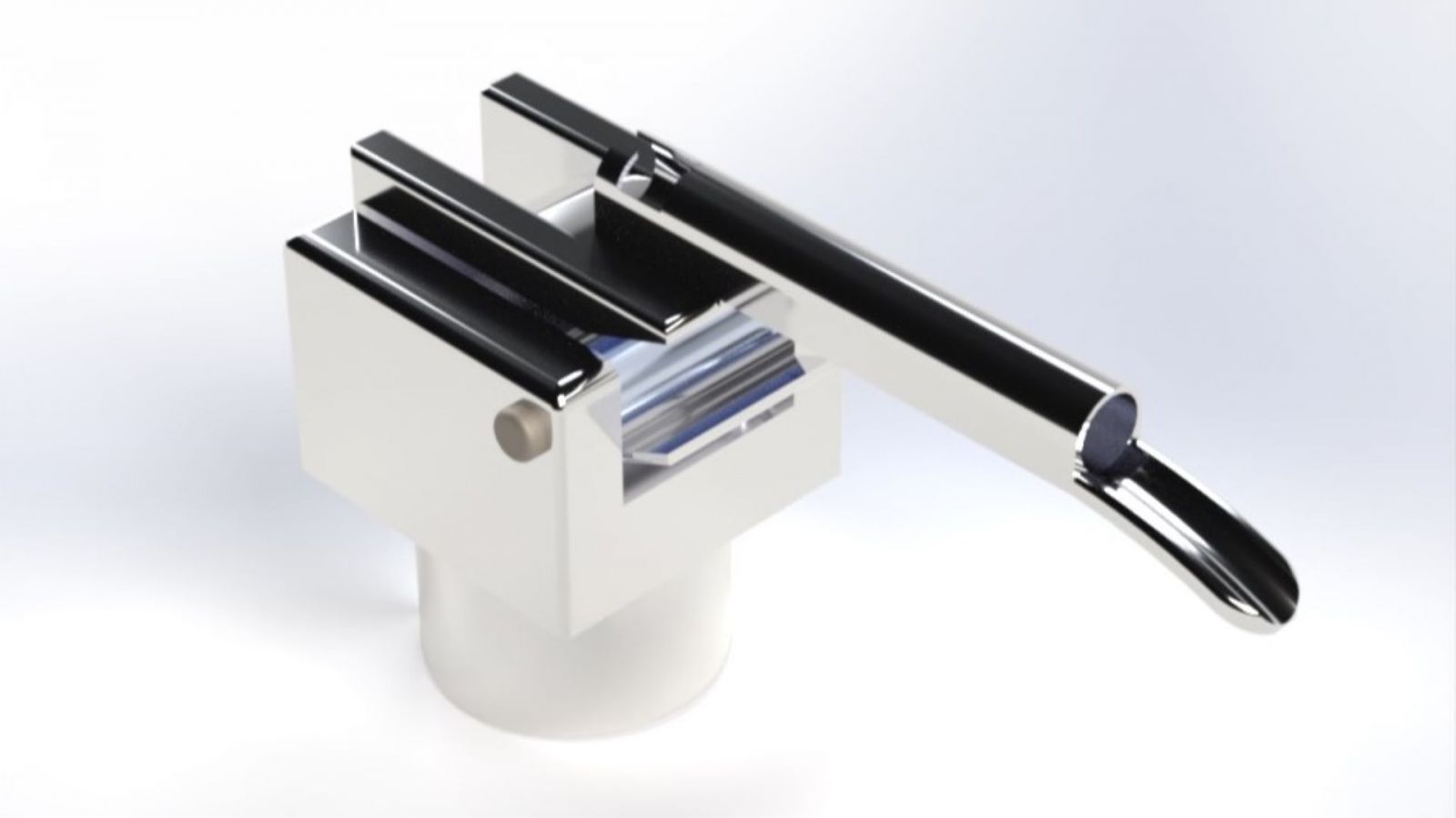
In the past year, Yearling’s capstone students have worked on designing and building low-cost oxygen concentrators, portable neonatal incubators, video laryngoscopes, neonatal cooling blankets, and continuous positive airway pressure (CPAP) devices. Their goal was to simplify the functionality of existing commercial devices without sacrificing quality.
Ekhaguere’s vision is to provide a set of devices that can be used independently and support neonatal care in regions where that care is limited or nonexistent. The MET student projects are designed to help close the health equity gap between high-income and low- to middle-income countries. As a result, he set design goals based on his experience in the field:
- The parts can be easily manufactured close to the location of use
- The parts and materials can be easily sourced worldwide
- The device can be easily assembled in the field, given reasonable instructions and skillset
- The device can be easily maintained in the field.
The capstone course required students to complete a design, build or manufacture the design, and verify the project based on a set of customer requirements. Between two and five students worked together on the fast-paced project for one semester. Throughout the development process, students received weekly feedback from Ekhaguere on function and design before the final devices would be tested, validated, and finally presented to clinicians who provide critical feedback on the work.
The class also visited an active NICU at Riley Hospital for Children, where they examined high-tech devices in the unit and interacted with NICU nurses and hospital biomedical engineers to understand the basic structure of the devices.
Ekhaguere says even though life-saving neonatal devices have improved significantly over the years, the benefits of those improvements have primarily benefited people in high-income countries, mainly because of the prohibitive cost of purchasing and maintaining these technologies. Paring down the devices to their essential features and functions not only makes manufacturing parts easier, but it makes neonatal technology easier to maintain in areas with limited resources and access.
“Although the core functions of these devices are basic—an incubator simulates the womb by providing heat and humidity—the need to appeal to the market in high-income countries results in devices being fitted with additional features that drive up cost and complexity but not the life-saving functionality,” Ekhaguere said.
“We believe there is a critical need to isolate core functionality, simplify technology and reduce the cost of essential neonatal technologies to make them more accessible in LMICs.”
Yearling has collaborated with Simon Cancer Center and IU Health on multiple undergraduate and graduate projects over the last five years, which led to this partnership with Ekhaguere for the MET capstone course. He believes students should be able to see the value of their work through high-impact projects that make a difference for people in need.
“With over 20 years of industry experience from the shop floor up, I think it is very important graduating MET students can apply what they have learned in their degree program to real-world problems,” Yearling said.
“My goal is to equip students with the skill set to operate effectively in a team, understand how to initiate a project, and complete the project successfully and on time. To achieve this goal, I am always seeking high-impact, worthwhile projects that engage students.”
This year’s projects are still a work in progress, according to Yearling and Ekhaguere. They are currently in the validation testing phase with the devices, including conducting in-vitro testing with premature lung simulators for a CPAP device and animal validation studies on the low-cost incubator and cooling blanket used to treat birth asphyxia in preterm and term newborn equivalent piglets, respectively. They have also requested ethical approval to conduct animal validation studies on the low-cost incubator and cooling blanket used to treat birth asphyxia.
“The students often take great pride and commitment to the project because of the noble cause behind it,” Ekhaguere said. “The students envision their work saving lives somewhere someday, and they are motivated to give their best.”
Additional information
- Mechanical Engineering Technology (degree page)
- Construction management student finds full-time job through program’s internship (Purdue Polytechnic newsroom)
- ‘Hands-on learning and practical experiences’ define Purdue for Indianapolis student (Purdue Polytechnic newsroom)
