The human body’s nervous system can be considered one’s personal networking system. If information needs to travel from one part of your body to another, it’s your nervous system that gets it there.
Researchers have been examining the nervous system for a means to remedy certain physical and neurological conditions through a treatment known as deep nerve stimulation (DNS). DNS uses electrodes that target the root of the nerve that is transmitting a corrupted data signal through the body’s network of nerves. The electrodes can then override the system with a corrected signal.
“A number of disorders, including migraine, rheumatoid arthritis and many gastrointestinal illnesses, can be treated with DNS,” said Robert Nawrocki, assistant professor in Purdue Polytechnic’s School of Engineering Technology. Nawrocki believes this direct approach to pain management and condition treatment is preferable to pharmaceutical treatments because, “compared to conventional chemical medicines, DNS can be applied directly where it is needed and avoid many side effects associated with chemicals, which need to first be dissolved in your stomach before only a fraction of that amount is delivered right where the problem is.”
 However, despite DNS’s potential for better patient outcomes, the process is not yet widely used because the electrodes that need to be applied to patients are not cooperating with the patients’ skin.
However, despite DNS’s potential for better patient outcomes, the process is not yet widely used because the electrodes that need to be applied to patients are not cooperating with the patients’ skin.
“Current techniques of DNS are typically invasive because the non-invasive electrodes available suffer from a number of disadvantages, including poor mechanical matching with soft skin tissue, poor spatial resolution and dermatological responses, precluding long-term use.”
Essentially, neurologists aren’t able to repair the body’s misfiring neurological “software” until improvements can be made to the DNS treatment’s hardware.
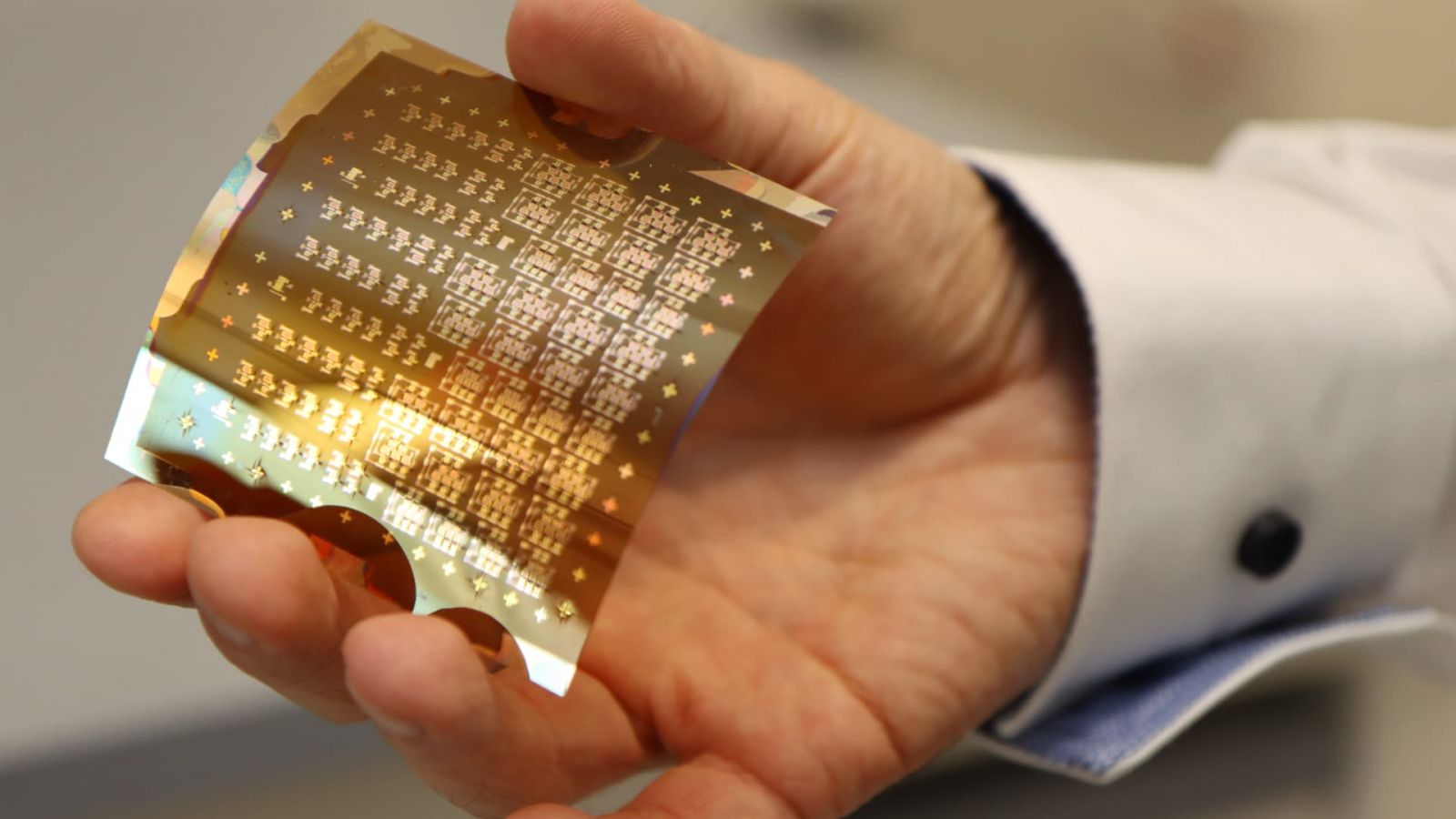
Enter Nawrocki’s research team. They want to develop “a subcutaneous, non-invasive, bi-directional neural interface in a wearable form factor for reliable and widely accessible neuromodulation treatment.” Or, in other words, they’re working on a soft, flexible electrode that can be placed on (or just below) the skin. The new electrodes will sense electrical activity from deep nerves and will stimulate those nerves with the correct electrical message without damage to human tissue or the electrodes.
Nawrocki said his new class of stretchable and breathable electrodes will offer higher effective surface areas and superior conformal skin contact, enabling long-term monitoring and deep nerve stimulation. The electrodes will be designed to provide signal-to-noise ratios that are superior to current state-of-the-art metal or gel silver/silver chloride electrodes for signal recording and nerve stimulation without allergic skin reaction. Furthermore, these electrodes will offer stretchability, gas (carbon dioxide) and liquid (sweat) permeability, enabling the skin to breathe, and ultrahigh conformability to irregular 3D skin surface, making the electrodes less noticeable and allowing for more long-term use.
To accomplish this research, Nawrocki has been awarded a Showalter grant. The Ralph W. and Grace M. Showalter Research Trust Fund was established to provide for medical and scientific research at Purdue University and Indiana University. The honor makes Nawrocki the first faculty member in Purdue University’s Polytechnic Institute to receive the award.
Collaborating with Nawrocki are Matthew Ward, research assistant professor in Purdue’s Weldon School of Biomedical Engineering, and David Bahr, professor and head of Purdue’s School of Materials Engineering.
